The Risks Associated with Hysterectomy: What You Need to Know

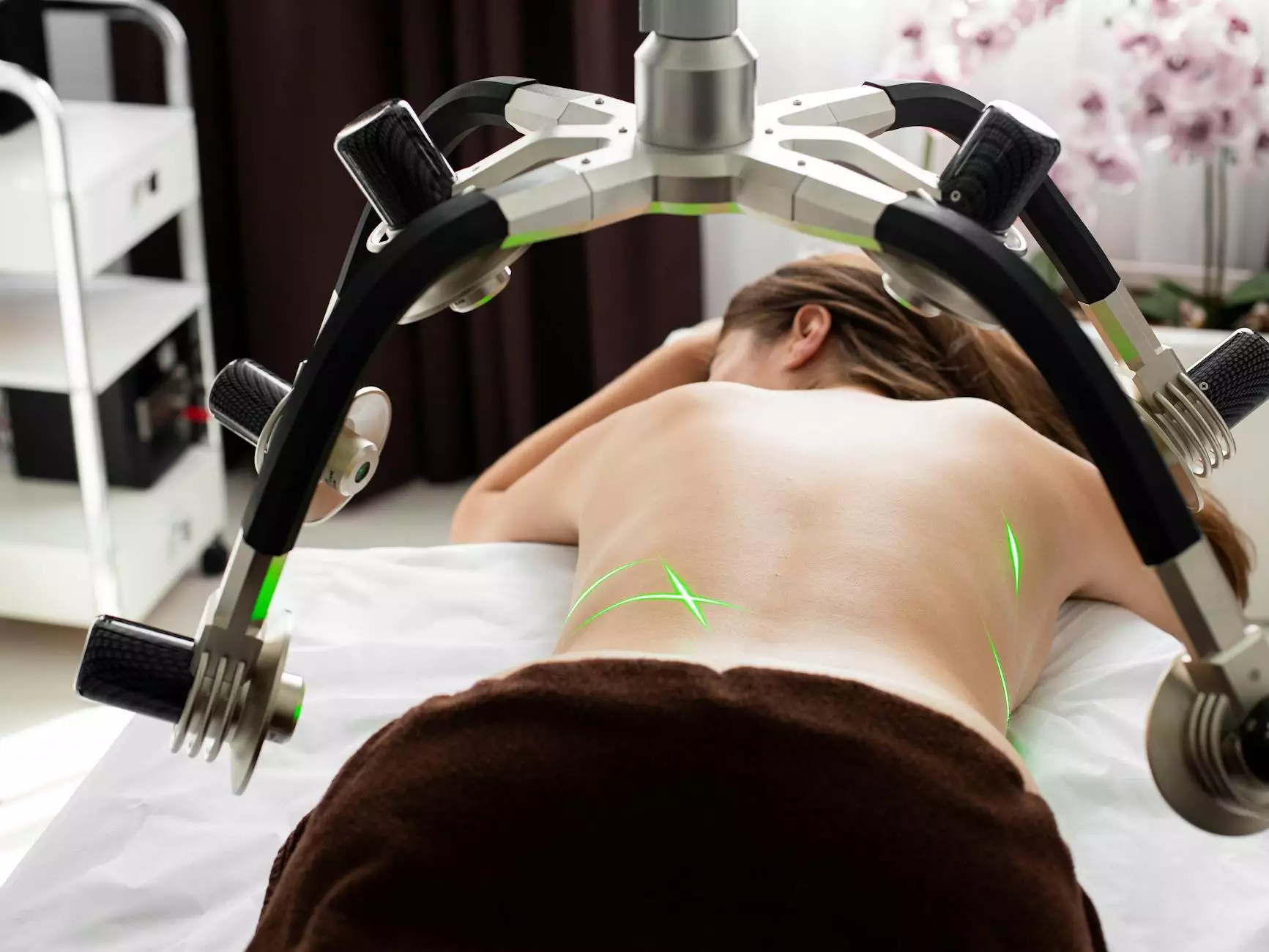
Deciding to undergo a hysterectomy is a significant choice for any woman, often necessitated by various medical conditions such as uterine fibroids, endometriosis, or abnormal bleeding. While the procedure can relieve many symptoms and improve quality of life, it is essential to be fully informed about the risks associated with hysterectomy. This article aims to explore in-depth the potential complications, the recovery timeline, and expert advice for anyone considering this surgery.
Understanding Hysterectomy
Before diving into the associated risks, it's crucial to understand what a hysterectomy entails. This surgical procedure involves the removal of the uterus and can be categorized into different types:
- Partial Hysterectomy: Removal of the upper part of the uterus while leaving the cervix intact.
- Total Hysterectomy: Removal of the entire uterus along with the cervix.
- Radical Hysterectomy: Involves the removal of the uterus, cervix, surrounding tissues, and part of the vagina; often performed in cancer cases.
Each type comes with its own set of potential benefits and risks. To make an informed decision, patients should consult with healthcare professionals to evaluate the best approach according to their medical history and current health status.
Potential Risks and Complications
No surgical procedure is devoid of risks. Understanding the risks associated with hysterectomy can help patients prepare for what lies ahead. Here are some of the potential complications:
1. Surgical Risks
Like any major surgery, hysterectomy carries inherent surgical risks, including:
- Infection: Post-operative infections can occur, sometimes requiring antibiotics or additional surgery.
- Bleeding: Excessive bleeding may necessitate a blood transfusion.
- Anesthesia complications: Reactions to anesthesia can occur, including respiratory issues or allergic reactions.
- Damage to surrounding organs: There is a risk of unintentional injury to the bladder, ureters, or intestines during surgery.
2. Hormonal Changes
For women who undergo a total hysterectomy, especially if the ovaries are removed, there can be significant hormonal changes. These can lead to:
- Menopause: Sudden onset of menopause can result in hot flashes, night sweats, and mood swings.
- Bone Health Risks: A decrease in estrogen levels may contribute to a higher risk of osteoporosis.
3. Long-term Health Risks
Research indicates that women who have undergone a hysterectomy may experience certain long-term health risks, including:
- Cardiovascular Disease: There is some evidence to suggest an increased risk of heart disease post-hysterectomy.
- Sexual Dysfunction: Changes in hormone levels and alterations in anatomy can lead to decreased libido or discomfort during intercourse.
- Pelvic Organ Prolapse: Surgery to remove the uterus can weaken pelvic support structures, potentially leading to prolapse.
Recovery Period Insights
Understanding the recovery process is equally as vital as knowing the risks. The recovery time after a hysterectomy varies based on the type of surgery (abdominal, vaginal, or laparoscopic) and individual health circumstances. Generally, one can expect:
- Hospital Stay: Typically, 1-3 days, depending on the surgical type and individual recovery.
- Initial Recovery: Most women can return to normal activities within 6-8 weeks, but this can vary.
- Follow-Up Appointments: Regular follow-ups are crucial for monitoring recovery and addressing any complications.
Best Practices for a Healthy Recovery
To enhance recovery post-hysterectomy, adopting certain practices can be beneficial:
- Rest and Relaxation: Allowing your body to heal by getting adequate rest is essential.
- Nutrition: A balanced diet rich in vitamins and minerals supports recovery and overall health.
- Physical Activity: Gradual reintroduction of light physical activity, as recommended by your doctor, can enhance recovery.
- Consult Healthcare Professionals: Always keep in touch with your healthcare team for advice tailored to your recovery journey.
Making Informed Health Decisions
Preparing for a hysterectomy means being aware of its benefits, the risks associated with hysterectomy, and the recovery path. Here are critical steps to ensure you make informed decisions:
- Seek Second Opinions: Consulting multiple healthcare providers can provide different perspectives and validated options.
- Educate Yourself: Familiarizing yourself with procedures and risks can alleviate anxiety and empower decision making.
- Discuss Concerns: Don’t hesitate to express concerns or ask questions regarding surgery and its implications.
Conclusion
While a hysterectomy can significantly improve quality of life for many women, it is imperative to understand the potential risks associated with hysterectomy. Every woman’s situation is unique, and each decision must be tailored to individual health needs with informed consent. Further research, doctor consultations, and personal reflections on the benefits versus the risks will pave the way for the most suitable healthcare path.
Remember, the journey doesn’t end at surgery; proactive post-operative care and ongoing lifestyle adjustments are vital for a healthy future. By prioritizing your health, you can navigate your recovery successfully and regain control over your well-being.